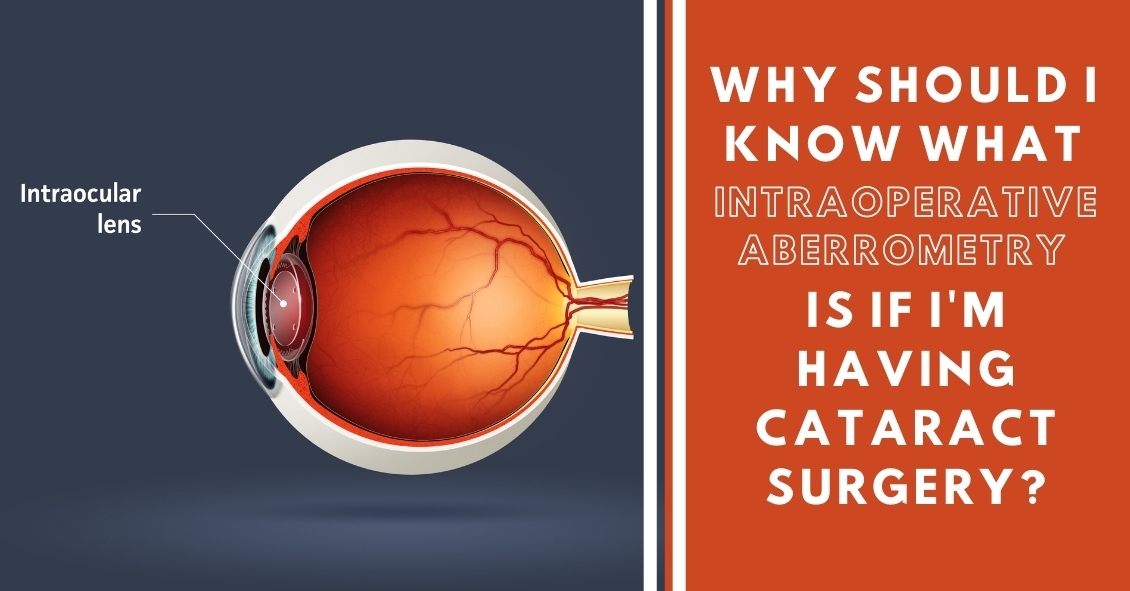
What Is Intraoperative Aberrometry?
Yes, that is a mouthful, but the concept isn’t quite as hard as the name.
An Intraoperative Aberrometer is an instrument we can use in the operating room to help us determine the correct power of the implant we put in your eye during cataract surgery.
Cataract surgery is the removal of the cloudy natural lens of your eye and the insertion of a new artificial lens inside your eye called an intraocular lens (IOL).
The cloudy cataract that we are removing has focusing power (think of a lens in a camera) and when that lens is removed, we need to insert an artificial lens in its place to replace that focusing power. The amount of focusing power the new IOL needs has to match the shape and curvature of your eye.
To determine what power of lens we select to put in your eye, we need to measure the shape and curvature of your eye prior to surgery. Once we get those measurements, we can plug those numbers into several different formulas to try and get the most accurate prediction of what power lens you need.
Overall, those measurements and formulas are very good at accurately predicting what power lens you should have. There are, however, several eye types where those measurements and formulas are less accurate at predicting the proper power of the replacement lens.
Long Eyes: People who are very nearsighted usually have eyes that are much longer than average. This adds some difficulty with the accuracy of both the measurements and the formulas. There are special formulas for long eyes but even those are less accurate than formulas for normal length eyes.
Short Eyes: People who are significantly farsighted tend to have shorter-than-normal eyes. Basically, the same issues hold true for them as the ones for longer eyes noted above.
Eyes with previous refractive surgery (LASIK, PRK, RK): These surgeries all change the normal shape of the cornea. This makes the formulas we use on eyes that have had previous surgery not work as well when the normal shape of the cornea has been altered.
This is where intraoperative aberrometry comes in. The machine takes the measurements that we do before surgery and then remeasures the eye while you are on the operating room table after the cataract is removed and before the new implant is placed inside the eye. It then presents the surgeon with the power of the implant that the aberrometer thinks is the correct one. Unfortunately, the power that the aberrometer selects isn’t always exactly right, but with the combination of the pre-surgery measurements and the intra-surgery measurements the overall accuracy is significantly enhanced.
The intraoperative aberrometry is also very helpful in choosing the power of specialty lenses like multi-focal and toric lenses.
We would encourage you to consider adding intraoperative aberrometry to your cataract surgery procedure if you have either a long or short eye (usually manifested as a high prescription in your glasses) or if you have had any previous refractive surgery.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
 Just like adults, children need to have their eyes examined. This need begins at birth and continues through adulthood.Following are common recommendat...
Just like adults, children need to have their eyes examined. This need begins at birth and continues through adulthood.Following are common recommendat...