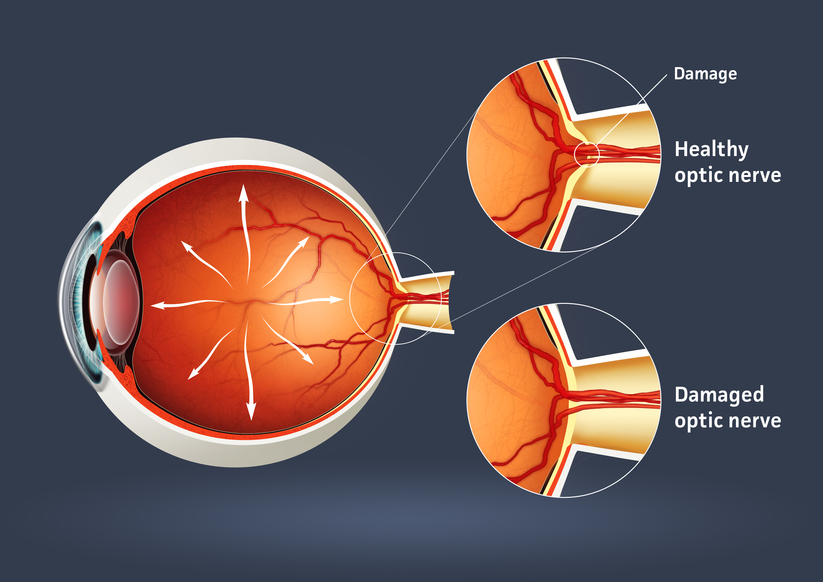
Glaucoma is a serious sight-threatening condition in which there is an abnormal pressure inside the eye. Typically, the pressure or IOP (intraocular pressure) is too high for the blood vessels and optic nerve to function normally, leading to loss of vision.
There are some forms of glaucoma that can occur with normal pressure in the eye. The average IOP for a healthy eye is 10 to 22 mm of Mercury. Just as a physician’s office tests your blood pressure annually, the eye doctor tests your IOP during annual eye examinations.
Types of Glaucoma
There are several varieties of the disease, with primary open-angle glaucoma being the most common. Primary open-angle glaucoma (POAG) occurs when the IOP is higher than normal. As the pressure increases, it destroys vital nerve tissue that is irreparable. POAG usually occurs over a long period of time, months to years, and slowly causes peripheral visual field loss. If left untreated, a sufferer progresses to tunnel vision and then to total blindness.
A second type of glaucoma is acute-angle closure. This is considered a medical emergency because the interocular pressure spikes suddenly to anywhere from 30-70 mm or higher. This causes extremely sharp pain, nausea and vomiting, and cloudy vision. The IOP needs to be lowered within hours to prevent permanent vision loss.
Juvenile open-angle glaucoma, or JOAP, is similar to POAG, in that is causes a gradual visual field loss. The most common form is in children from ages 3 to 21. Infantile or congenital glaucoma is a type of glaucoma that manifests itself between birth to 3 years of age. A typical sign is an enlarged bluish-gray cornea, the front dome of the eye. Excessive tearing of the eye and sensitivity to light are also symptoms. Finally, secondary glaucoma is caused from trauma, eye disease, or certain medications.
Causes of Glaucoma
Many theories on the cause of glaucoma exist, but the exact cause is unknown. Glaucoma can be a hereditary condition. It also can be caused by malformed anatomical structures in the eye. Certain risk factors such as hyperopia and cataracts cause a higher incidence of certain types of glaucoma.
One cause of glaucoma is an insufficient drainage system of the aqueous fluid. The aqueous imbalance causes a gradual buildup of pressure which destroys vision. Another cause is an insufficient flow of blood to the optic nerve. Ocular trauma or injury that damages the anterior segment for the lens and drainage mechanism of the eye can also lead to glaucoma. In the case of normal tension glaucoma, pressure readings are in the normal range. The cause of this is unknown.
Treatment
Even though in most cases there is no way to prevent glaucoma, there are many treatment options. Medications in the form of eyedrops are commonly prescribed. Different combinations of agents act on mechanisms of action to lower IOP or to slow the production of fluid.
Advanced surgical and laser procedures can also be viable options for the treatment of glaucoma. An in-office procedure called laser trabeculoplasty can cause the meshwork in the eye to work more efficiently. This treatment has a temporary effect and may need to be done multiple times. Another effective surgery uses a drainage implant to facilitate better outflow and inflow of aqueous fluid in the eye. These procedures help keep the pressure stabilized. Conventional surgery for glaucoma is done in an operating room scenario. A flap in the eye is created to facilitate outflow of the pressure. This pressure-controlling surgery is known as a trabeculotomy.
Furthermore, some oral medications can also be used in the treatment of glaucoma.
Methods of Testing for Glaucoma
During a comprehensive eye examination, eye pressure can be tested through various methods. Tonometry gives a pressure reading of the eye. A tomometer has different methods such as a probe that gently touches the front of the eye after the eye doctor has administered anesthetic eyedrops. Another method of testing uses a puff of air. For children, there is a tonometer that is quick and does not require anesthesia.
A pachometer, which measures the thickness of the front of the eye called the cornea, can also aid in diagnosis. A visual field device can measure for early or late damage in the peripheral fields of vision. Lastly, newer technology called OCT, or optical coherence tomography, counts the nerve fibers, which can help detect early changes in the disease.
Prevalence of Glaucoma
There are approximately 3 million individuals in the United States with glaucoma. It is the second leading cause of blindness in the country. Most cases are found in the population over age 40, and more women than men have the disease. Two thirds of glaucoma cases are in the Caucasian population, approximately 20% are African-American, and 10% are Hispanic. Glaucoma continues to rise every year in the population.
The key to success in the treatment of glaucoma is early detection and progressive monitoring of the condition. Comprehensive eye examinations and diligent monitoring will help protect from vision loss with this disease.
Citations
- Glaucoma. AOA pdf. AOA.org.
- I Care Tonometry in Children. JAAPOS. Sciencedirect.com. April 2011
- Glaucoma, open -angle. NEI source press release. 2010.
 Recent Census Bureau data shows a population of approximately 71 million baby boomers (the generation born from 1946-1964). What does that...
Recent Census Bureau data shows a population of approximately 71 million baby boomers (the generation born from 1946-1964). What does that...